Gestational Hypertension: Protecting Mothers and Babies
Gestational hypertension, a pregnancy-related condition, is characterized by high blood pressure that develops after the 20th week of gestation, potentially posing risks to both the mother and the developing fetus.
Unveiling the Silent Threat: How Gestational Hypertension Poses Risks During Pregnancy
Expecting mothers face numerous challenges during pregnancy, and one of the most common yet often overlooked conditions is gestational hypertension. Did you know that gestational hypertension affects 1 out of 11 pregnant women in India [1]?
This article will explore the world of gestational hypertension, its prevalence, impact, signs, detection, and potential complications.
Gestational Hypertension
Gestational hypertension (GH) is defined as systolic blood pressure of 140 mm Hg or higher and/or diastolic blood pressure of 90 mm Hg or higher after 20 weeks of pregnancy, without proteinuria or liver/kidney problems [2]. In a reassuring development, mothers generally experience a notable resolution of gestational hypertension within a span of 12 weeks or less following delivery [4].
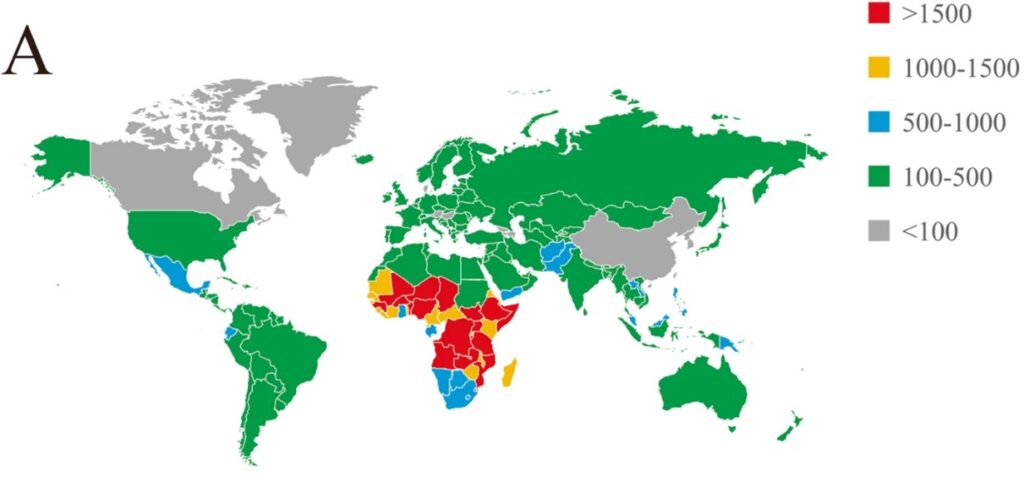
Gestational Hypertension: An Overview of Prevalence and Impact
Gestational hypertension represents a significant global concern, with a prevalence ranging from 1.8% to 4.4% of pregnancies worldwide [4]. It is of utmost concern, however, that this condition contributes to maternal mortality rates of 10-15% on a global scale [3]. Its prevalence in India is estimated at 5% (95% CI, 4%–6%) [1]. Therefore, understanding its prevalence and impact is crucial for raising awareness and taking proactive measures to protect mothers and babies.
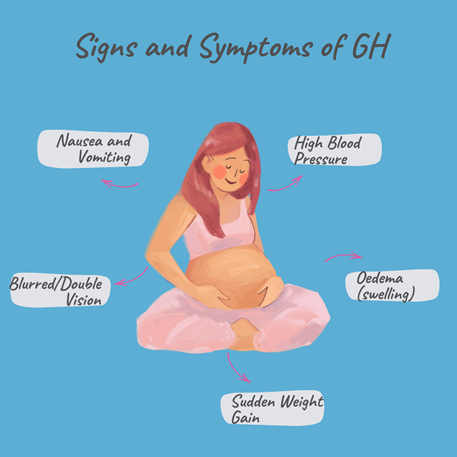
Recognising the Signs and Symptoms of Gestational Hypertension
Clinical Detection of Gestational Hypertension: Essential Tests and Evaluations
If one experiences any of the above symptoms (Figure 1), they should visit the doctor promptly. The doctor may conduct a comprehensive evaluation, including a detailed medical history and will regularly monitor the patient’s blood pressure (B.P. ≥ indicates Gestational Hypertension). Moreover, GH in mothers can also pose a threat to the fetus’s well-being and lead to fetal distress. Hence, regular fetal monitoring is also done to rule out fetal complications. Other essential tests (urine dipstick test, USG, blood tests, Doppler studies etc.) are also prescribed to rule out the possibility of complicated conditions such as preeclampsia. eclampsia, placental abruption and stroke (the placenta separating from the uterus wall), which arises from long durations of high blood pressure.
Factors Increasing the Risk of Gestational Hypertension
Several factors can increase the risk of developing gestational hypertension. These include having a clinical history of chronic hypertension, diabetes type 1 or 2, or kidney disease. Furthermore, other factors such as carrying multiple babies, being younger than 20 or older than 40, and obesity may also increase the chances of developing hypertension in pregnancy [7].
What are the Potential Complications of Gestational Hypertension? (Understanding the Dangers)
Gestational Hypertension can have serious complications. Increased blood pressure can damage the blood vessels and hamper blood flow to the brain, kidneys, uterus, placenta, and liver. Moreover, it can lead to serious conditions such as preeclampsia, eclampsia, and heart disease. These serious conditions can cause placental abruption (early separation of the placenta from the uterus wall), seizures, poor fetal growth and development, premature births, and even death of mother and baby [6].
Studies indicate that women with GH diagnosed after 36 weeks of gestation have about a 10% risk of developing PE [9] and approximately 10-15% of women with GH progress to developing preeclampsia on a global level [8].
Early Detection and Effective Management: How do they help safeguard maternal and Fetal Health?
Timely detection of GH helps the doctor make better decisions about managing the condition and preventing complications. It is essential to attend all prenatal doctor appointments so that any variations in blood pressure can be kept in check.
The doctor will suggest diet changes and regular blood pressure checks if a confirmed diagnosis of Gestational HTN is made. Low-dose aspirin [7] or lifestyle changes such as exercise and sleeping may also be prescribed.
Limitations and Future Directions
While we have learned much about gestational hypertension, there is still more to discover. Extensive research has shown that gestational hypertension runs in families; however, the genes responsible for it have not been identified [11]. It is hoped that as the cause becomes known, more targeted approaches and medications can be developed to deal with gestational hypertension and other hypertensive disorders.
Additionally, the mechanism of progression from gestational hypertension to preeclampsia has not been explained. Further research and statistics are needed to paint a complete picture of how many lives are lost to hypertensive disorders each year, especially in India.
Join Us in Raising Awareness
As mentioned above, gestational hypertension is a silent threat that can pose significant risks to both mothers and babies. We can safeguard maternal and fetal health by recognising the signs and symptoms, understanding the importance of clinical detection, and taking proactive steps for early management. Let us join hands in raising awareness and empowering pregnant women to protect themselves and their precious little ones from the potential dangers of gestational hypertension. We will discuss preeclampsia and its management.
Remember, maternal and fetal health matter. Together, we can make a difference!
References:
[1] Dhinwa M, Gawande K, Jha N, Anjali M, Bhadoria AS, Sinha S. Prevalence of hypertensive disorders of pregnancy in India: A systematic review and meta-analysis. J Med Evid 2021;2:105-12
[2] CDC. (2023, June 19). High blood pressure during pregnancy. Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/pregnancy.htm
[3] Sadanandan, K.1; Kurian, S.2; Valliot, B.2; Sasidharan, A.1; Sherin, N.1; Madhu, R.1; Ramesh, S.1; Mondain, S.3. PREVALENCE OF GESTATIONAL HYPERTENSION AND FACTORS INFLUENCING SELECTION OF ANTI-HYPERTENSIVE DRUGS IN PREGNANCY. Journal of Hypertension 37():p e239-e240, July 2019. | DOI: 10.1097/01.hjh.0000573064.05528.af
[4] Umesawa, M., Kobashi, G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res 40, 213–220 (2017). https://doi.org/10.1038/hr.2016.126
[5] The Children’s Hospital of Philadelphia. (2014, August 23). Gestational hypertension. Chop.edu. https://www.chop.edu/conditions-diseases/gestational-hypertension
[6] Gestational Hypertension1. (2010). In Obstetric Clinical Algorithms: Management and Evidence (pp. 24–25). Wiley-Blackwell.
[7] Geddes, J. K. (2017, May 3). Gestational Hypertension. What to Expect; WhattoExpect. https://www.whattoexpect.com/pregnancy/high-blood-pressure/
[8] Preeclampsia and gestational hypertension. (2019, February 5). Division of Cardiology. https://www.columbiacardiology.org/patient-care/womens-heart-center/about-heart-disease-women/pregnancy-and-heart-disease/preeclampsia-and-gestational-hypertension
[9] Saudan P, Brown MA, Buddle ML, Jones M. Does gestational hypertension become pre-eclampsia? Br J Obstet Gynaecol. 1998 Nov;105(11):1177-84. doi: 10.1111/j.1471-0528.1998.tb09971.x. PMID: 9853766.
[10] Wang, W., Xie, X., Yuan, T. et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population‐based study. BMC Pregnancy Childbirth 21, 364 (2021). https://doi.org/10.1186/s12884-021-03809-2
[11] Williams PJ, Broughton Pipkin F. The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011 Aug;25(4):405-17. doi: 10.1016/j.bpobgyn.2011.02.007. Epub 2011 Mar 22. PMID: 21429808; PMCID: PMC3145161.