Exploring the Significance of Preeclampsia Beyond Pregnancy
The Lifelong Impact of Preeclampsia: Understanding Long-Term Effects on Mothers and Offspring
Imagine this: You’re in the middle of an incredible journey called pregnancy, eagerly anticipating the arrival of your little one. But suddenly, preeclampsia barges in and throws everything off balance. Preeclampsia is an unwelcome guest that arrives after the 20th week of pregnancy, bringing high blood pressure and organ failure to moms-to-be. Shockingly, it affects 2-8% of women worldwide [18]. It’s not just a temporary setback during pregnancy; it can cast a long, dark shadow over the lives of both the mother and the baby.
This blog explores preeclampsia’s long-term effects and implications, shedding light on its significance beyond the immediate pregnancy period.
Understanding Preeclampsia
Preeclampsia (PE) is a rapidly-progressing hypertensive disorder (high blood pressure) of pregnancy. It can be potentially fatal for both the mother and baby [2]. In India, it develops in 0.3 to 25.8% of pregnancies [19].
In our previous blog, we discussed the causes, diagnosis, appropriate management to minimise the impact on the mother and foetus and much more about the condition. In this blog, we will move forward to discuss what its long-term impact is.
Preeclampsia’s Impact on the Mother
Immediate health risks during pregnancy
Preeclampsia can cause complications such as early delivery, HELLP syndrome, placental abruption, and eclampsia (coma and seizures) [1]. Although Preeclampsia is confined to pregnancy, its consequences can manifest up to 15 years later [4].
Long-term health complications for mothers
Cardiovascular health implications
Preeclampsia has been linked to a significant fourfold rise in the likelihood of developing heart failure in the future. Additionally, it carries a twofold increased risk of coronary heart disease, stroke, and mortality due to coronary heart or cardiovascular disease. The elevated risk of heart failure, stroke, and cardiovascular disease-related mortality is more pronounced within the initial ten years following a pregnancy complicated by preeclampsia than the risk beyond the 10-year mark [10].
Increased risk of hypertension and heart disease
Preeclampsia increases the risk of chronic hypertension. It also lowers the age at which hypertension onset happens – exposing mothers to more extended periods of organ damage [4].
Other complications
Post a preeclamptic pregnancy, the risk of end-stage renal disease (ESRD) in later life is 5-12 times [3,5]. The main kidney problem after preeclampsia is focal segmental glomerulosclerosis (scar tissue in the kidney’s filtering unit that can lead to kidney failure), often linked to chronic hypertension [6].
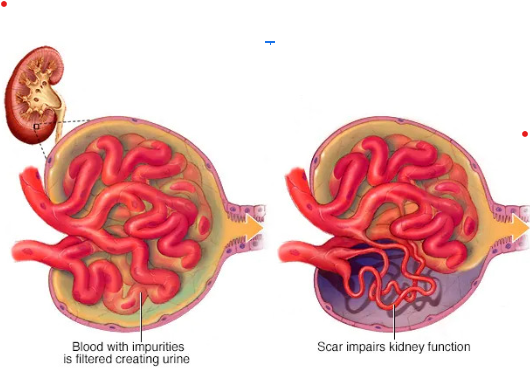
Fig 1.
Focal segmental glomerulosclerosis
Before the onset of cardiovascular and renovascular diseases, there may be signs of underlying health issues such as obesity, problems with blood vessels, increased resistance in blood vessels, insulin resistance, and high levels of lipids in the blood (dyslipidemia). These conditions can progress to hypertension, diabetes, thyroid disease, and kidney problems, which are more likely to occur after experiencing preeclampsia. Ultimately, this can lead to premature coronary artery disease, kidney disease, and a shorter lifespan [6].
Emotional and psychological effects
Beyond the physical implications, addressing the potential impact of preeclampsia on mental health is crucial. Preeclampsia is linked to an increased risk and severity of cognitive impairment, psychosocial distress, and psychiatric disorders like depression, anxiety, and post-traumatic stress disorder. Research suggests that certain substances released by the preeclamptic placenta, such as anti-angiogenic factors and pro-inflammatory cytokines, can harm the blood-brain barrier endothelium. This damage can cause long-term structural and functional changes in the brain, potentially contributing to mental health problems [11].
Preeclampsia’s Impact on the Baby
Foetal Development and Growth Issues
Children born to mothers with a history of preeclampsia face increased health risks. Preeclampsia often leads to intrauterine growth restriction (IUGR) and premature birth, contributing to long-term health issues.
Some studies have found negative correlations between preeclampsia and subsequent cardiovascular and neurological health of the offspring [12].
One study also describes the differential impact of preeclampsia on babies depending on their sex. The study found that preeclampsia (PE) exposure during foetal life negatively affects linear growth. However, in girls, positive associations with weight and BMI were observed. These findings emphasise the significance of the foetal period in terms of growth and support the idea that an unfavourable intrauterine environment can impact postnatal development [13].
Premature birth and associated complications
Doctors may advise early delivery of the baby to minimise the damage caused by preeclampsia to the mother and baby. Premature births increase the risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy [14].
Increased risk of chronic conditions in childhood and adulthood
IUGR alone is a risk factor for hypertension and cardiovascular diseases [7]. Even infants born from preeclamptic pregnancies with more than 2.5 kg weight experience higher systolic blood pressure as they grow into children and adolescents [8]. Follow-up studies have shown that the offspring of non-severe preeclampsia have a relative risk of 1.8, while severe preeclampsia increases the relative risk to 2.2 for developing strokes [9].
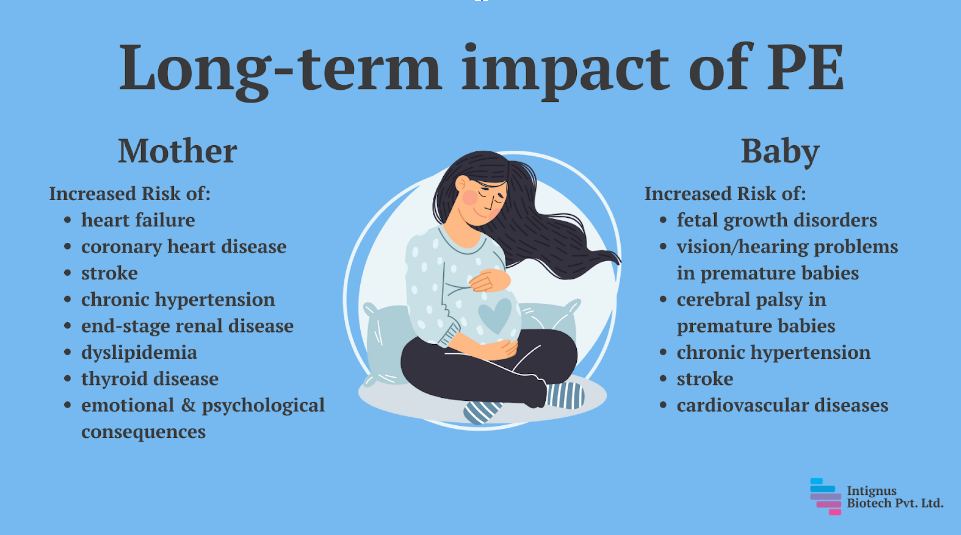
Fig 2.
The long-term impact of PE on mother and baby
Strategies for Managing and Preventing Long-Term Consequences
Management of preeclampsia involves three key aspects: prevention, early detection, and treatment [16].
There is limited evidence to support interventions like rest, exercise, reduced salt intake, garlic, marine oil, antioxidants, progesterone, diuretics, and nitric oxide as preventive measures for preeclampsia (PE). However, low-dose aspirin, particularly when started before 16 weeks in high-risk groups, and calcium supplementation, especially in populations with low intake, hold promise for preventing PE [15].
Antenatal care for high-risk women involves regular check-ups, blood pressure and urine checks, growth assessments, and foetal monitoring. Baseline investigations are essential for monitoring and include various blood tests and vital sign measurements [16].
Delivery is the only cure for preeclampsia, with the timing based on maternal stabilisation and foetal well-being. Postpartum follow-up is crucial to monitor blood pressure and assess long-term risks. Recurrence of preeclampsia and associated testing may be relevant for future pregnancies [16].
Ushma Patel’s Encounter with Long-Term Effects of PE
Ushma Patel shared the story of her VBAC (vaginal birth after caesarean) after a brain haemorrhage from preeclampsia. Ushma had a normal pregnancy up to 35 weeks when she began experiencing symptoms of severe Preeclampsia and partial HELLP syndrome. A week later, she delivered early and was put on magnesium sulphate to prevent seizures [17].
After spending a few days in the hospital, surrounded by nurses and doctors, she and her daughter were diagnosed with several complications. Ushma was diagnosed with a subarachnoid brain haemorrhage (bleeding in the space surrounding the brain), and her daughter had developed jaundice, and the doctors suspected a murmur, too. The doctors determined Ushma’s haemorrhage was due to the high blood pressure she endured due to Preeclampsia [17].
When they were discharged a couple of days later, Ushma struggled with breastfeeding and bonding with my baby, as well as postpartum depression and PTSD from the traumatic delivery. Her daughter had difficulties gaining weight and was diagnosed with a congenital heart defect at four months. After open heart surgery at seven months and eye surgery at 15 months, she was diagnosed with Noonan Syndrome in 2016 [17].
Ushma had another baby after a few years. This time, she knew what to watch out for and had a smoother experience. She delivered naturally without major complications and is the mother of two lovely children today [17]. Having another pregnancy without major complications after PE is possible!
Conclusion
Prioritising ongoing care and support is crucial for managing the long-term effects of preeclampsia. Regular monitoring, lifestyle modifications, and addressing mental health concerns through counselling are essential. Healthcare providers should collaborate across specialities to implement comprehensive management strategies and ensure the well-being of those affected. With continuous monitoring, education, and support, we can minimise the long-term impact of preeclampsia, enabling healthier and happier lives for mothers and their children.
References:
[1] Preeclampsia. (n.d.). Cleveland Clinic. Retrieved July 13, 2023, from https://my.clevelandclinic.org/health/diseases/17952-preeclampsia
[2] Atlantic Health System. (2019, September 19). 10 things women should know about preeclampsia. Newswise. https://www.newswise.com/articles/10-things-women-should-know-about-preeclampsia
[3] Rachel Mathew, Benita P. Devanesan, Srijana, N.S. Sreedevi, Prevalence of hypertensive disorders of pregnancy, associated factors and pregnancy complications in a primigravida population, Gynecology and Obstetrics Clinical Medicine, Volume 3, Issue 2, 2023, Pages 119-123, ISSN 2667-1646, https://doi.org/10.1016/j.gocm.2023.01.002.
[4] Turbeville, H. R., & Sasser, J. M. (2020). Preeclampsia beyond pregnancy: Long-term consequences for mother and child. American Journal of Physiology-Renal Physiology. https://doi.org/F-00071-2020
[5] Paauw, N. D., Luijken, K., Franx, A., Verhaar, M. C., & Lely, A. T. (2016). Long-term renal and cardiovascular risk after preeclampsia: towards screening and prevention. Clinical science (London, England: 1979), 130(4), 239–246. https://doi.org/10.1042/CS20150567
[6] Williams D. (2011). Long-term complications of preeclampsia. Seminars in nephrology, 31(1), 111–122. https://doi.org/10.1016/j.semnephrol.2010.10.010
[7] Barker, D. J., Osmond, C., Golding, J., Kuh, D., & Wadsworth, M. (1989). Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. British Medical Journal, 298(6673), 564-567.
[8] Davis, E. F., Lazdam, M., Lewandowski, A. J., Worton, S. A., Kelly, B., Kenworthy, Y., … & Leeson, P. (2012). Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics, 129(6), e1552-e1561.
[9] Kajantie, E., Eriksson, J. G., Osmond, C., Thornburg, K., & Barker, D. J. (2009). Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki birth cohort study. Stroke, 40(4), 1176-1180.
[10] Wu, P., Haththotuwa, R., Kwok, C. S., Babu, A., Kotronias, R. A., Rushton, C., Zaman, A., Fryer, A. A., Kadam, U., Chew-Graham, C. A., & Mamas, M. A. (2017). Preeclampsia and future cardiovascular health: A systematic review and meta-analysis: A systematic review and meta-analysis. Circulation. Cardiovascular Quality and Outcomes, 10(2). https://doi.org/10.1161/CIRCOUTCOMES.116.003497
[11] Srajer, A., Johnson, J. A., & Yusuf, K. (2022). Preeclampsia and postpartum mental health: mechanisms and clinical implications. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 35(25), 8443–8449. https://doi.org/10.1080/14767058.2021.1978067
[12] Lu, H. Q., & Hu, R. (2019). Lasting Effects of Intrauterine Exposure to Preeclampsia on Offspring and the Underlying Mechanism. AJP Reports, 9(3), e275. https://doi.org/10.1055/s-0039-1695004
[13] Byberg, K. K., Øymar, K., Eide, G. E., Forman, M. R., & Júlíusson, P. B. (2017). Exposure to preeclampsia in utero affects growth from birth to late childhood dependent on child’s sex and severity of exposure: Follow-up of a nested case-control study. PLoS ONE, 12(5). https://doi.org/10.1371/journal.pone.0176627
[14] Preeclampsia. (2022, April 15). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745
[15] Moura, H., Lopes, L. M., Murthi, P., & Costa, S. (2012). Prevention of Preeclampsia. Journal of Pregnancy, 2012. https://doi.org/10.1155/2012/435090
[16] English, F. A., Kenny, L. C., & McCarthy, F. P. (2015). Risk factors and effective management of preeclampsia. Integrated Blood Pressure Control, 8, 7-12. https://doi.org/10.2147/IBPC.S50641
[17] Website. (n.d.-d). Preeclampsia – VBAC after brain hemorrhage from preeclampsia. Preeclampsia Foundation – Saving Mothers and Babies from Preeclampsia. Retrieved July 13, 2023, from https://www.preeclampsia.org/our-stories/vbac-after-brain-hemorrhage-from-preeclampsia
[18] WHO recommendations for Prevention and treatment of pre-eclampsia and eclampsia.
[19] Dhinwa M, Gawande K, Jha N, Anjali M, Bhadoria A, Sinha S. Prevalence of hypertensive disorders of pregnancy in India: A systematic review and meta-analysis. Journal of Medical Evidence. 2021;2(2):105.